-
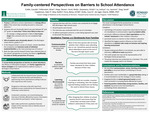
Family-Centered Perspectives on Barriers to School Attendance
Cassidy Cottle, Brian A. Fellenstein, Steven M. Hepp, Molly Hurd, Kristin Karpowicz, Joshua H. Le, Jasmine M. Liu, and Sarah Yang
Background: Truancy, or chronic absenteeism, is defined as missing 10% or more of school days. Students who are chronically absent any year between 8th and 12th grade are seven times more likely to drop out. A Howard Center survey found that 33% of students in the Burlington school district were chronically absent. Schools identified the complex and intensive needs of students and families as the main driver of truancy. Our aim was to survey family perspectives on barriers to school attendance, the efficacy of attempted strategies, and family suggestions for future strategies to address truancy in Chittenden school districts.
Methods: We designed an interview script that was used to interview families recruited by community partners. Eight coders examined interview notes using a thematic content analysis to identify areas of need for families.
Results: We conducted a group interview of four Somali families via translator. Themes from caregivers’ responses included: 1) communication breakdown between the school and families, 2) racism as perceived systemic bias from school staff, 3) safety as a perceived lack of concern by the school for students, and 4) caregivers identified the biggest positive influence on their child’s attendance as teachers who create an inclusive and inspiring learning environment.
Conclusion: More work is needed to learn the diverse perspectives of the Burlington community. Families may be more comfortable with group interviews conducted at established, school-sponsored events. Based on the interviews, fostering positive relationships among teachers, families, and students may prove to be most beneficial at combating chronic absenteeism.
-
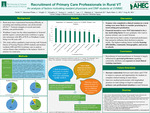
Recruitment of Primary Care Professionals in Rural Vermont: An analysis of factors motivating resident physicians and DNP students at UVMMC
Tanner L. Ferrell, Julia Halvorson-Phelan, Christopher Kruglik, Anton Krutyakov, Angelina Kuzina, Anna Landis, Joon Young Lee, and Kathleen Waeldner
Background: Windham Aging was created to analyze, primarily, ways for senior residents to age in place; a November 2022 report concluded that one of the barriers is lack of primary care professionals. The current physician workforce is aging into retirement with 48% of PCPs in Windham County being over 60 years old. Previous literature reported the following themes among primary care professionals as factors in determining retention and recruitment: financial, social, lifestyle, and community.
Methods: This research study aimed to identify strategies to enhance the recruitment of primary care professionals in rural areas of Vermont. The study team conducted interviews with family medicine residents and Doctor of Nursing Practice (DNP) students. Using a qualitative, inductive approach, the team identified key themes that could impact the recruitment of primary care professionals in rural Vermont, including a 5-point scale on previously identified factors affecting recruitment.
Results: Trainees (n=13) ranked housing, political association, community factors, and access to schools as most important. Qualitative analysis revealed that trainees’ financial incentives weigh less heavily than previous rural clinical experience and interest in living in a rural setting.
Conclusion: Recruitment of rural practitioners in Vermont is largely influenced by personal preferences regarding community attributes and exposure to rural clinical training experience.
-

Improving Access to Adult Home-Based Palliative Care Through Medicaid Expansion
James T. Go III, Adam M. Lewis, Rachel E. Miles, Surya Radhakrishnan, Shruthi Santhanakrishnan, and Anthony M. Vejar
Background: Palliative care is associated with a more than fifty percent reduction in costs associated with end-of-life care. Currently 30% of Vermonters receive their healthcare through Vermont’s state Medicaid program. Despite this large proportion of Medicaid recipients, there is no Medicaid-funded home-based palliative care program in the state. The objective of this project is to better understand the need for home-based palliative care and assess the barriers to these services.
Methods: A systematic literature review was conducted to develop a palliative care service package based on the models of Arizona, California, and Hawaii. Interviews with medical professionals and a focus group with representatives from multiple Home Health Agencies (HHAs) were conducted. The interviews and focus group were recorded and transcribed. Transcripts were reviewed by two separate coders in NVivo software, and the codes reconciled to unify qualitative themes and quotes.
Results: From qualitative data, several core themes were extracted such as: benefits to healthcare, staffing and reimbursement, and education. Overall, benefits to providers and patients and educational gaps were among the most emphasized themes. Staffing and reimbursement were the primary concerns for HHAs for whom fee-for-service models may not be sufficient.
Conclusion: Implementation of home-based palliative care services can benefit patients and healthcare providers by reducing hospitalizations and enhancing patient care. Delivery of these services remains challenging due to a variety of factors, including financial and staffing constraints from HHAs and educational gaps within the healthcare community. Medicaid expansion may help ensure effective palliative care delivery in Vermont.
-

Assessing College-Age Adult Attitudes and Perceived Barriers and Facilitators to HPV Vaccination
Arman S. Grewal, Katina Messier, Christopher Pham, Aina K. Rattu, Susanna L. Schuler, Deepinder Singh, Peter Vien, and Abigail B. Wootton
Background: The HPV vaccine is recommended for people aged 11 to 26 and is effective at preventing against certain types of cancers. Current vaccination rates among college-aged individuals remain inadequate. This study aims to assess attitudes to HPV vaccination and elucidate differences in awareness among individuals of different vaccination status.
Methods: Medical students and premedical undergraduate students engaged individuals in a central campus student location to collect survey responses and educate about HPV and HPV vaccination. A peer-education approach was utilized to engage students. Knowledge gaps were generally assessed via a true/false questionnaire during peer-to-peer interactions and a link to a REDCap survey was shared. Respondents completed it themselves. We used one-way ANOVA and T-tests to compare levels of awareness levels and HPV vaccination status.
Results: 209 survey responses from UVM students qualified for analysis. A majority of students had completed an HPV vaccine series. Survey results showed respondents learned of HPV and the vaccine from a variety of sources, but primarily from family or in a clinical setting. Average awareness also varied amongst individuals with differing HPV vaccination status.
Conclusion: There may be associations linking greater knowledge of HPV with “Completed” vaccination status. Results demonstrate that awareness may not equate to general knowledge of HPV, possibly contributing to disparities in vaccination rate. With year-to-year HPV vaccine awareness declining, there is an increased need for educational campaigns to not only raise awareness about HPV but also on HPV topics like its transmission, disease prevention, and federal guidelines.
-

Improving Health Communication: Testing Preferences and Choices for Health Information to Improve Literacy
Casey Norton, Wendy Memishian, Sarah Kohl, Kyle M. Gorman, Muhammad H. Zeb, Haziq Aziz, Taylor Lamarre, and Adam B. Thompson
Background: Health literacy and effective health communications are growing areas of concern. This project aims to determine differences in health literacy and preferred communication methods of health information between Vermont rural and urban populations.
Methods: In-person surveys were conducted in Vermont rural and urban settings. Clinical trials were used as a baseline example of health communication to gather information on preferred methods of receiving health information, and comfort interpreting health information. Survey questions were developed using pre-established questionnaire guidelines from CDC health status surveys. Statistical analysis was performed using Microsoft Excel and GraphPad Prism 6. Chi-squared and unpaired T-tests were used for data comparison.
Results: 272 individuals completed the initial survey with 262 meeting inclusion criteria. Of the 262 respondents, 89% white (n=233) and 54% female (n=141), 55% had a bachelor’s degree or higher (n=145); 14.5% reported having previously participated in a clinical trial (n=38). Distribution of zip codes based on Rural-Urban Commuting Area (RUCA) Codes showed individuals from rural area populations (RUCA = 10) and metropolitan area core populations (RUCA = 1). Survey results found statistical significance between rural and urban populations in comparing health communication preferences, with rural participants significantly preferring television and social media as outlets to receive health information.
Conclusions: Both urban and rural residents most frequently selected healthcare providers as a preferred communication outlet, followed closely by the internet. Mean confidence level differences between rural and urban populations for multiple modalities of medical information were not statistically significant.
-

Inclusive Sexual History for Sexually and Gender Diverse Individuals in Vermont
Krystal Ramos-Barrera, Kimberly Michelle Jones, Elizabeth Karakashian, Ian Minearo, and Ashley Lucero
Background: Patients that identify as lesbian, gay and/or transgender (LGBTQ+) experience poorer healthcare outcomes due to discrimination, stigma, and marginalization. Interaction with a new healthcare environment is through intake forms which often use hetero-centric language around sexual history gathering. We address this by the assessment of these forms through the lens of members of the LGBTQ+ community. We aim to decrease the harm associated with current wording and improve the experience and trust of patients who identify as sexual or gender diverse.
Methods: We used focus groups as our primary means of data collection. First, we recruited a group of participants based on our research objectives. Second, we conducted 2 focus group sessions totaling 6 participants in a private setting and took detailed notes. Third, we analyzed the data using thematic analysis and 5 people coded the data into categories. Then, we visualized the findings using quotes and summarized the main themes. Finally, we presented the survey of updated questions to guests at the LGBTQ+ Health Summit to gain feedback.
Results: Thematic analysis of the focus group data demonstrated multiple prominent themes. These themes reflected gender and sexually exclusive word choices, phrasing that was exclusive to patients for which English is not a primary language, and lack of question clarity.
Conclusion: Despite major advancements in the quality of care LGBT+ patients receive in the primary care setting, there are still considerable adjustments that need to be made to ensure all individuals feel respected and included while giving a sexual history.
-
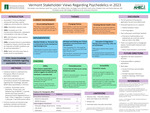
Vermont Stakeholder Views Regarding Psychedelics in 2023
Cole Zweber, Josephine Yalovitser, Sarah Tran, Lauren Tien, Mallory Stultz, Ava Siegel, Henry M. Mitchell, and Jonah Levine
Background: Psychedelics, such as MDMA, LSD, ketamine, and psilocybin, are defined as mind-manifesting substances. While Indigenous communities have used psychedelics for millennia, scientific research in the United States began in the 1940s. Following a rise in recreational psychedelic use during the Counterculture Movement of the 1960s, many psychedelics were issued Schedule I status. In the past fifteen years, research on the therapeutic potential of psychedelics has emerged as a burgeoning field. The objective of this study was to assess opinions towards psychedelics in Vermont.
Methods: Using a literature review on psilocybin, MDMA, LSD, ketamine, and ayahuasca, an interview guide was designed to explore current attitudes on the state of psychedelics, policy surrounding psychedelics, and ongoing training and treatment practices. A convenience sample of 16 healthcare providers, legislators, investors, advocates, and law enforcement officers was interviewed.
Results: Qualitative analysis of interview transcripts indicated a need for superior pharmacologic treatment to address the growing mental health crisis and expressed cautious optimism with regards to the promise of psychedelics. Interviewees emphasized the importance of further research on efficacy and safety and expressed concerns for current models of legalized psilocybin. Counselor training and education emerged as crucial considerations for psychedelic treatment. Other barriers included cost, scalability, and equitable access.
Conclusion: While the growing body of research on psychedelics indicates promise in addressing intractable mental health disorders, voices from all sides advise the field to exercise caution. Further research is needed to ensure equitable access, establish safe treatment procedures, and enact responsible policies.
-

Behind Closed Doors: Substance Use Disorder and Human Trafficking in Vermont
Arif S. Ahsan, Adaugo Chikezie, Jordan S. Franco, Heather A. Kettlewell, Caitlin E. Marassi, Dan J. Mitchell, and Kae L. Ravichandran
Background: Human trafficking is a humanitarian crisis. Current literature identifies risk factors predisposing individuals to becoming trafficked, including housing insecurity, substance use disorders, and disrupted childhood households. This study investigates the relationship between human trafficking and substance use disorder in Vermont.
Methods: Nine qualitative interviews were conducted with professions directly interacting with victims of human trafficking in Vermont, representing Law Enforcement, Healthcare, and Community Services professionals. A standardized interview guide included questions that aimed to uncover risk factors, health and support needs, and challenges victims face. Two coders individually reviewed each set of interview notes prior to meeting to finalize themes and subcategories, to construct a thematic network.
Results: Substance use was cited as strongly associated with human trafficking by each category of professionals, and several additional themes emerged. Accessibility to resources was cited twice as frequently as the next most common theme, the nature of human trafficking, with subcategories of limited ability to help victims and victim’s lack of transportation most frequently mentioned. The nature of human trafficking theme included sex work/trafficking and Vermont-specific issues as the most frequent subcategories, while complex medical issues and socioemotional concerns shared the third most cited theme.
Conclusion: Human trafficking and substance use disorder are closely entwined in Vermont. To address this public health crisis, national guidelines should be augmented with regional risk factors and accessibility concerns. Additional research must be conducted to expand this Vermont specific data set. Risk factors and accessibility concerns in Vermont should be compared to other regions in the United States.
-

Using Telehealth to Meet the Unique Needs of Rural Communities
Lindsay Aldrich, Jack J. Braidt, John S. Burke, Ryan P. Kelly, Kelly J. Knight, Elizabeth M. O'Neill, Virginia S. Ramirez, and Gabriela F. Sarriera-Valentin
Introduction: Many Vermonters report difficulties in accessing healthcare, and telehealth became a widespread solution during the COVID-19 pandemic. The continued use of telehealth may improve health disparities for Vermonters. The objective of this study was to investigate perspectives on telehealth among patients and healthcare providers.
Methods: A cross-sectional survey-based study design was used. Provider surveys were distributed via e-mail and patient surveys were distributed via Front Porch Forum throughout Vermont. A major limitation of the study is that this was a convenience sample and may not equally represent all Vermont practitioners and patients.
Results: Scheduling appointments was 2.04 times easier for those with private insurance vs public insurance (P< 0.05), and was 2.57 times easier for those < 60 years old compared to those ≥60 years old (P< 0.01). There were no statistically significant differences between Chittenden County and the remainder of Vermont. 73% of providers agreed that telehealth has led to improvements in patient outcomes, and pediatricians were twice as likely to be satisfied with their patient interactions via telehealth.
Conclusion: Overall, most patients in our study were satisfied with their telehealth interactions (72%) and agreed that telehealth expanded their access to healthcare (60%). The lack of significant differences in our study between Chittenden County and the remainder of Vermont may be due to variations in public/private insurance, internet access, and specialists under-utilizing telehealth. The biggest concerns among respondents were the lack of physical exams via telehealth, which could be addressed through patient and provider education and the use of at-home technologies.
-
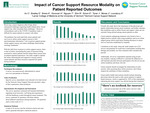
The Impact of Resource Modality on Reported Outcomes in Cancer Patients
Clemens An, Ellie Bradley, Katelynn Briere, Hannah Donovan, Tin Nguyen, Edward Simon, Jennifer Toner, and Bryan Shin
Background: The state of Vermont is one of the most rural states in the nation as more than 80% of people live in either rural areas or small cities. This provides a unique challenge for cancer survivors in Vermont to find and access appropriate forms of support. With the shift towards virtual medicine due to COVID, cancer survivors had to significantly adapt to new restrictions which hindered their ability to find resources for emotional support and information. Due to these circumstances, we wanted to identify the trend in usage and efficacy of various modalities for support by cancer survivors.
Methods: Cancer survivors completed an online opt-in self-reported survey regarding which resources they accessed and their experiences during their cancer treatment. The goals of this study were to identify prominent informational and supportive sources accessed by cancer patients, compare the frequency with which cancer patients used online versus in-person resources, evaluate the impact each resource had on patient outcomes, and elucidate optimal strategies of disseminating crucial information to cancer survivors.
Results: We hypothesized that online resources would have the highest rates of usage, while in-person support networks would result in greater efficacy. Based on the results (n=20), more people utilized in-person resources, and in-person resources were associated with more favorable patient outcomes.
Conclusion: This study revealed that cancer patients utilized in-person resources, such as relationships with healthcare professionals and support networks, more often than online resources. The use of these in-person resources was correlated with higher average patient emotional well-being and level of informedness.
-

How Vermont State Legislative Health Leaders Prioritize Community Health Needs: A Qualitative Analysis
Anayis M. Antanesian, Sarah Caffry, Nicolas Hutt, Andrew Leckerling, Jiayi Luo, Kadi Nguyen, Anthony Quach, and George Zhang
Background: The Affordable Care Act requires hospitals to develop Community Health Needs Assessments (CHNAs) every 3 years, identifying community-specific health goals and implementation strategies. However, it is unclear how CNHAs are translated into healthcare policy. College of Medicine students analyzed how Vermont state legislative health leaders prioritized community health needs and their alignment with hospital CHNAs.
Methods: The Senate Committee on Health and Welfare participated in a virtual focus group; all five committee members were asked six questions by a student moderator. The session was transcribed and corroborated with video review. Utilizing qualitative analysis, responses were independently reviewed and coded into common themes to identify trends in health priorities as identified by the policymakers, and Senators’ methods used to identify those health needs.
Results: Community health priorities identified by Senate health policymakers aligned with many reported in CHNAs, although CHNAs were not used in their decision-making process. All Senators cited mental health services, affordable housing, and substance use; categories also listed in the top five needs by most Vermont hospital CHNAs.
Conclusion: This study found that top health priorities of Senate health policy leaders align with CHNAs. While policymakers did not prioritize use of CHNAs as a resource to inform decision-making, CHNAs may provide a beneficial resource for them moving forward. For example, childcare and obesity often appear in CHNAs, but were not highlighted in the focus group. Future broader studies may give a more comprehensive understanding of potential CHNA utility in real-world health care policy development and implementation.
-
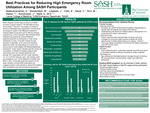
Best Practices for Reducing High Emergency Room Utilization Among SASH Participants
Anupama Balasubramanian, Max Breidenstein, Jacob P. Cappiello, Bradford R. Clark, Chellam E. Nayar, McLaine S. Rich, and Taylor R. Walker
Background: SASH is a Vermont-based health promotion program that aims to provide affordable housing and care for older Medicare recipients. SASH organizes programs including monthly events, learning presentations, group physical activities, and blood pressure clinics. Through these programs and with the support of their care nurses, SASH has significantly reduced overall Medicare expenditure for their participants, but high-ED utilizers remain a population in which further intervention can decrease costs and resources.
Methods: This project used statistical analysis of SASH patient data for variables of interest to examine the leading reasons for high ED utilization among SASH participants, then explored ways to address these issues with a literature review. These programs were then compared to existing SASH programs, and based on this comparison, recommendations were made on ways that SASH can address frequent ED usage among its participants.
Results: SASH patients had a median of seven visits throughout the duration of data collection. Issues related to hypertension, type 2 diabetes, and falls were leading causes of high-ED utilizer visits.
Conclusion: This study determined that there are several feasible programs that SASH can implement to decrease ED utilization among its participants, including: utilizing a screening questionnaire to connect patients with PCPs and flag high-risk patients, training nurses to assist with blood glucose monitoring and fall prevention education, expanding monthly health events (eg. technology literacy workshops), creating educational videos on falls prevention and healthy diet planning, and expanding food and exercise support to include activities like field trips to the grocery store.
-
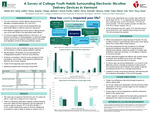
A Survey of College Youth Habits Surrounding Electronic Nicotine Delivery Devices in Vermont
Emily C. Battle, Caitlin Early, Audree Evans, Stefanie Geiger-Kelsey, Callan Gravel-Pucillo MMS, Anirudh A. Hirve, Caleb P. Maness, and Dhiraj Patel
Background: Teen e-cigarette use increased between 2017 and 2019; however, youth perceived that non-cigarette tobacco products were less addictive than traditional cigarettes, when in fact many vaping devices contain more nicotine than cigarettes. Although vaping in middle and high school students has been extensively studied, data surrounding undergraduates is lacking.
Methods: The present study surveyed undergraduate students from three Vermont colleges. Of the 326 respondents, 147 reported vaping at some point in their life. The survey was created using RedCap and analysis was conducted using SPSS.
Results: The reported mean age of vaping initiation was 16.5 ± 2.1 years. Of all participants who had ever vaped (n=147), 61% reported trying to quit at some point, 25% reported never trying to quit, and 14% failed to answer the question. Of the respondents who vaped within the last 30 days (n=74), 77.1% obtained vaping products from a physical store, 20.0% from friends, 1.4% online, 1.4% from another provider not listed, and 0.0% from family. A significant association was found between a history of vaping and agreement with the statement: “it’s cool to vape on campus” (X2: (2, N= 320) = 20.968, p< 0.001).
Conclusions: Although participants commonly cited friends as a reason for initiating vaping, many denied feeling direct peer pressure to vape. Students reported being more likely to vape at school than at home. Additionally, the most common method reported of purchasing devices was through physical stores. Future research should identify effective strategies to assist youth struggling to quit and reduce underage purchasing in physical stores.
-

Improving Blood Donation Rates through Analysis of Motivational Factors for Repeat and New Black Donors
Jasmine A. Bazinet-Phillips, Ashfi Chowdhury, Olivia Darko, Michelle Falcone, Benjamin M. Glickman, Alec M. Schrager, and Tyler VanDyk
Background: During the COVID-19 pandemic, vaccination clinics held in community centers provided a solution for increasing vaccination rates in the Black community Blood donations, like vaccination turnouts, could correlate with accessibility of donation center location. Our project asked new and recurrent Black blood donors, about their donation preferences to identify recruitment solutions.
Methods: An eighteen-question, online-anonymous survey, was distributed to American Red Cross (ARC) blood donors who self-identify as African American and have donated > 1 time since 1/1/2019. Responses from 512 blood donors were received regarding their knowledge of sickle cell disease, frequency of donation, familiarity with the donation venue, their preferred informational medium, and motivations for donating. Responses collected 4/20/222 - 4/27/22 were stratified into “repeat donors” (>3 times since 2019, n=329) and “new donors” (< 3 times since 2019, n=183).
Results: New donors who preferred to donate blood at a community center (28.0%) were more likely to co-select “giving back to [their] community” as a primary motivation (80.8%, p = 0.048). New donors also indicated “walk-in” scheduling preference compared to recurrent donors (54.8% vs 42.8%, p= 0.032), whereas recurrent donors demonstrated significant preference for scheduling “>1 month in advance” (22.6% vs 42.2%, p < 0.0001). Additionally, new donors were unsure of where to donate blood as compared to recurrent donors (11.3% vs 3.8%, p=0.009).
Conclusions: The study results indicate that consideration should be given to disbursement of information regarding the location of the venue and scheduling options for blood drive participants.
-
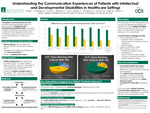
Understanding the Communication Experiences of Patients with Intellectual and Developmental Disabilities in Healthcare Settings
Ty E. Bever, Olivia Dominque, Charlotte Evans, Aathmika Krishnan, Michael H. Le, Ashwini Sarathy, Rachel Thompson, and Richard Q. Vuong
Background: Recent studies demonstrate that individuals with intellectual and developmental disabilities (IDD) face communication challenges in healthcare settings. To evaluate the efficacy of communication between healthcare providers (HCPs) and individuals with IDD in Vermont, we surveyed and interviewed HCPs, direct support professionals (DSPs) and individuals with IDD.
Methods: We used a mixed methods approach to evaluate communication challenges patients with IDD face. Surveys were distributed to HCPs, DSPs and individuals with IDD. The surveys indicated the communication strategies preferred by each group and measured the experience level of HCPs and Ds working with individuals with IDD. Individuals with IDD and Ds were interviewed. Quantitative data were compared using non-parametric tests, with linear regression identifying factors related to patient comfort. Qualitative data were categorized by common themes.
Results: 91 surveys were completed by 18 DSPs, 2 individuals with IDD, and 71 HCPs. The proportion of HCPs with >5 years of experience working with IDD patients was significantly higher than DSPs (90.1% vs 66.7%, p=0.003). However, 55.6% of DSPs reported witnessing communication challenges between individuals with IDD and HCPs. The proportion of HCPs that routinely ask patients with IDD how they best communicate was significantly lower than the proportion of DSPs willing to share this information (50.7% vs 91.7%, p=0.010).
Conclusion: Despite high levels of provider experience, communication in the healthcare setting remains challenging for individuals with IDD. Areas for improvement include targeted interventions such as personalized communication tools and patientcentered approaches. HCPs must address these factors to improve quality of care for individuals with IDD.
-

Primary Care Provider and Medical Student Knowledge and Attitudes Regarding Cannabis in Vermont
Seth Brownmiller, Ana Homick, William Hsu, Clara Maxim, Leland Nguyen, Annie Penfield-Cyr, Serra Sozen, and Eric Stoutenburg
Background: There is growing debate about the use of cannabis containing products and community implications. Current research emphasizes determining the impact cannabis has on the short and long-term health of an individual. Our research was focused on the perception of cannabis use between medical students and primary care providers (PCPs).
Methods: We used an anonymous, 5-point scale survey to assess the knowledge and attitudes about cannabis use, including thoughts on Vermont’s upcoming adult use marketplace. Key emphasis was placed on the attitudes of public health, driving safety, effectiveness for medical conditions, and patient education.
Results: Roughly 64% of respondents believe cannabis may negatively affect public health, yet 90% of students and 58% of PCPs support the creation of an adult use marketplace. This is especially interesting to consider when an overwhelming majority of both students and PCPs agreed that alcohol use had a negative impact on public health. Confidence in patient education was also evaluated, which demonstrated an opportunity for both medical students and PCPs to receive additional training on the positive and negative impacts of cannabis to share with patients.
Conclusion: It is our goal that this work be used to further the conversation both inside and outside our healthcare system to better understand the public perception on cannabis, and the impact its use may have on the people in our communities. We hope this project will inspire future collaboration with the VT Cannabis Control board to serve as a source of valuable information about healthy policy surrounding cannabis use.
-

Weight Bias in Medical Students and Healthcare Professionals
Vyha T. Do, Jharna Jahnavi, Ryan Kamkar, Dana L. Kramer, Casey Krueger, Karena P. Nguyen, Vennela Pandaraboyinau, and Neeki Parsa
Background: Weight bias in healthcare leads to poorer communication, misdiagnoses, and less time spent with higher BMI patients. A gap in the literature exists for characterizing weight bias in healthcare. Our study aims to understand weight bias in local practitioners and medical students. We explore awareness of bias, confidence in navigating bias, and potential interventions to reduce the impact of weight bias
Methods: The 8-item Beliefs About Obese Persons questionnaire and adapted Attitude Towards Obese Patients and Perceived Weight Bias in Health Care questionnaires were distributed to medical students and physicians via email lists.
Results: 136 responses from preclinical students (n=73), clinical students (n=26), and physicians (n=22), were analyzed with paired t-tests. Physicians had the least amount of bias, followed by preclinical and then clinical students. Physicians were more likely to believe weight bias is an issue and be confident in their ability to navigate bias than preclinical students.
72.1% of all survey respondents indicated that weight bias is a problem. Open-ended field questions were coded and indicated that more training is needed, that weight bias exists in healthcare, and that bias is difficult to discuss. Respondents chose workshops as an effective intervention.
Conclusion: In our study, physicians showed the least bias, followed by preclinical students. Our results suggest longitudinal clinical exposure may help mitigate weight bias. Many participants regard weight bias to be present and concerning and view existing methods as ineffective. This study will inform future weight bias interventions to ensure improved outcomes for patients.
-
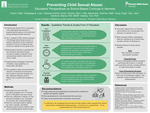
Preventing Child Sexual Abuse: Educators' Perspectives on School-Based Curricula in Vermont
Kate A. French, Luke Giangregorio, Annie Glessner-Fischer, Zachary Kramer, Casey Little, Matthew R. Rzemien, Paige Song, and Jessica Wyn
Background: Child sexual abuse (CSA) is associated with longitudinal repercussions in academic performance and physical and psychological health outcomes (1). Vermont passed Act 1 in 2009 aiming to mitigate the incidence of CSA via school-based curricula. Act 1 requires each district to have organized training on CSA for its employees and lessons for students at every grade level (2). This project surveyed six schools in Vermont to evaluate how districts have aimed to meet the mandate, obstacles they have encountered, and subjective efficacy of their current program.
Methods: Individuals involved with CSA prevention programs from six VT schools (preK-8th grade) were interviewed. Interviews addressed 1) efficacy of CSA prevention program in use, 2) parental involvement, and 3) general thoughts. Interview transcripts were coded to identify key concepts and beliefs. Lastly, codes were grouped into minor themes, which were assessed and compared to establish overarching themes.
Results: Many of the CSA programs addressed inappropriate behavior, standing up for yourself, sexuality, and the fear of speaking out. Shared obstacles for the schools included: time restriction in student and educator schedules, financial barriers including the cost of purchasing an effective program and hiring staff to teach it, and lack of parental involvement.
Conclusions: This study explored how six Vermont school districts have incorporated CSA education in response to Act 1. Overall, the educators expressed a dire need for a state-sponsored and standardized curriculum that is relatable for students and regularly updated, strict specifications for who should teach the curriculum, and clarity on the parental and/or community involvement.
-

Why 21?: Strategizing Substance Use Prevention
Elizabeth Kelley, Jessica Lucas, Tyler McGuire, Hunter Myers, Brittney Palermo, Marwan Ramadan, Javier Rincon, and Faith Robinson
Abstract
Background: Substance use in adolescence is associated with the development of substance use disorder. This study evaluates communication strategies and attitudes among caregivers/guardians and adolescents regarding substance use in adolescence to inform an upcoming campaign aimed at delaying substance use in the Winooski School District (SD).
Methods: Surveys targeting Winooski SD middle- and high-school students and caregivers/guardians were developed to assess understanding of the legal age of substance use and preferred sources of health information. Surveys were disseminated from March-May 2022 via Front Porch Forum, community dinners, newsletters, and school communications.
Results: The most common source of information about COVID-19 (a proxy for health information) that students reported was their parents (60%). Other common sources included friends (40%), doctors (40%), internet search (40%) and other (40%). Caregivers were most likely to report the CDC (62.5%) and other (62.5%) as sources of health information, with school communications (50%) and doctors (50%) also common. Caregivers and students most often select scientific (66%) and medical (25% reasons as the basis for the legal age of substance use being 21 years old. Respondents also cited the law (33% of caregivers and 12.5% of students) as a driving reason, and a similar proportion of respondents did not know the reason.
Conclusion: Given these findings, substance use prevention and education programs for adolescents may consider including parent participation with healthcare provider guidance. Improved survey distribution strategies with attention toward the unique demographics of Winooski are needed to increase survey response rates and offer more representative findings.
-

Assessing Cancer Prevention Knowledge During COVID-19 Pandemic
Robert Anthony Adamian, Lily Deng, Nicholas W. Krant, Trevor AR McDonald, Natalie Qin, Ally Sarkis, and Althea Jem Darbin Tapales
In response to the COVID-19 pandemic, adjustments in the provision of health care resources have caused a significant decrease in cancer screenings. These missed screenings may have considerable impacts on patients, health care practitioners and health systems.
In addition to the importance of resuming timely screening, studies have shown that a large portion of cancer deaths stemming from breast, skin, and colorectal cancer are preventable by risk factor modification at the patient level.
Many people remain uncertain of how best to prevent cancers, despite general awareness of concerns.
Raising awareness can empower patients to reduce their risk factors for developing breast, skin and colorectal cancer.
It has been shown that increased knowledge of colorectal cancer screening leads to increased participation in early screening, which can lead to better overall outcomes.
-

Initial Assessment of a Suicide Prevention Resource for Vermont Primary Care
Sam Afshari, Eliot Binkerd-Dale, Zain Chaudry, Varun Gupta, Morgan Howlett, Colleen McCarthy, Benjamin N. Price, and Rebecca B. Rawlings
Suicide is the second leading cause of death for Vermonters ages 10-44. Studies have shown that of those who die from suicide 45% have seen their primary care provider in the month prior to their death and only 20% saw a mental health provider.
To help strengthen suicide risk screening in primary care, a group of Larner College of Medicine students partnered with Chittenden Accountable Community for Health to curate a suicide prevention informational resource to be used in Vermont's primary care practices to promote universal suicide screening.
We then surveyed users of the tool to assess its utility and identify barriers to suicide screening within their practices.
-

Age Well: Home Health Care Shortages in Northwestern VT during the COVID-19 Pandemic
Jeremy Altman, Matthew Breseman, Edom Alemayehu Girma, Alexander M. Kubacki, Louisa Moore, Amanda Nattress, Noah Sorkow, and Kristen Wright
As of February 2021, there have been over 26.6 million cases and over 450,000 deaths in the United States due to COVID-19. Since the outbreak, a critical focus in the healthcare system has shifted towards protection of healthcare providers as well as vulnerable patients such as the elderly. The growing shortages of providers has resulted in a growing need for home health care (HHC). Beyond HHC addressing this workforce gap, evidence has shown a reduction in emergency department (ED) visits, hospital admissions and a 14- million-dollar savings in healthcare cost. While the role of HHC has been crucial for the efficacy of the healthcare system, like many other sectors, the COVID-19 pandemic has resulted in unforeseen challenges. According to a 2020 survey conducted by Home Health Care News, 92% of HHC agencies have lost a substantial amount of revenues due to shortage of resources in addition to an increase in patient and caregiver anxiety.
-

Motivators for Convalescent Plasma Donors during the COVID-19 Pandemic
Betsy Assoumou, Natalie J. Bales, Amy K. Chang, Hannah K. Cook, Kiana Heredia, and Colby J. Fischer
This study will seek to explore the motivators for convalescent plasma donors during the COVID-19 pandemic.
In 2020, the global pandemic caused by SARS-CoV-2 increased donations of transfusion products, particularly convalescent plasma from COVID-19 survivors that is used to provide passive antibody immunity to those infected. Convalescent plasma therapy has been identified as one of the only therapies for COVID-19 beyond supportive care.
Much of the current research focuses on the current motivators of whole blood and plasma donations, commonly citing altruistic motivations, knowing someone who has previously donated, and social media influence as common motivators for donations.
It is important to explore not only what motivates COVID-19 survivors to initially donate plasma, but also the motivations of repeat donors. By gaining a greater understanding of what these motivators are, we may be able to convert these convalescent plasma donors to regular blood donors.
-

Addressing Food Insecurity Within New American Communities in Vermont
Lorena Ayoub, Carl W. Brasch, Aria Elahi, Justin L. Esteban, Juwairiyyah Fatima, Brianna J. Spano, Sean Wang, and Erik J. Zhang
Food insecurity is defined as not having safe, nutritious, or culturally appropriate foods available, or having limited ability to acquire these foods/uncertainty as to when one can acquire these foods.
Reasons for food insecurity can be multifactorial such as language barriers, unfamiliar foods, and limited information about food environments.As a result, many turn to processed and energy- dense foods, contributing to the development of chronic diseases.
Food banks and local food shelves provide supplemental food assistance to residents and communities in need. However, with diverse New American populations living within the same community, it is challenging to determine which foods best fit their needs.
Vermont has welcomed 535 refugees in the last 4 years. Many of these new Americans currently reside in Winooski and Burlington. This study seeks to address the issues of mental health, food insecurity, access to the food shelf, and food preferences within the New American communities located in Winooski, Vermont.
-

Perceptions of Mask Use During the COVID-19 Pandemic
David Bachoy, Clara Berard, Nicholas D. Brunette, Sadie M. Casale, Tonya Conley, Krystal Gopaul, Tyler Landman, and Rhys Niedecker
The CDC recommends covering of the face and nose during the COVID-19 pandemic as a primary mitigation strategy for viral transmission. Masks minimize the number of viral particles emitted by the wearer; mask use serves to reduce the effects on population transmission.
Mask wearing behaviors have been shown to vary across different groups like gender identity, however, differences between people with and without lung disease have yet to be explored.
Goal: Examine perceptions, attitudes, and behaviors related to mask use during the COVID-19 pandemic of those with and without lung disease nationally.
All posters from the UVM Larner College of Medicine Public Health Projects, 2008 to present.
Printing is not supported at the primary Gallery Thumbnail page. Please first navigate to a specific Image before printing.

